Cluster A. Cardiovascular/Respiratory/Metabolic Diseases
Long-term Changes in Autonomic & Metabolic Function
Collaborative Project A1
Susan Redline, MD, M.P.H. (Project leader)
Harvard Medical School (Boston, MA)
Michael C.K. Khoo, Ph.D. (Primary BMSR Liaison)
This project represents the continuation of a long-standing collaboration that has enabled the development and testing of improved methods for assessing cardiovascular autonomic function across sleep-wake states in polysomnographic studies. Having found previously a significant association between autonomic dysfunction and impaired glucose metabolism, the overall goal of this project is to determine whether specific noninvasive measures of autonomic function, coupled with information about current status of glucose metabolism, are capable of predicting the progression of metabolic dysfunction. The specific aims of the project are to determine, using longitudinal data, whether:
- Long-term (~5 years) changes in heart rate variability (HRV) and pulse transit time variability are correlated with changes in glucose metabolism;
- Sleep-disordered breathing alters the association between long-term changes in autonomic and metabolic function.
- Baseline measures of cardiovascular variability and insulin resistance predict subsequent changes in diabetes status.
Model-based Approaches for Therapeutic Management of Neonatal Cardiovascular Abnormalities
Collaborative Project A2
Istvan Seri, MD, Ph.D. & Shahab Noori, MD (Project leaders)
Children’s Hospital of Los Angeles (Los Angeles, CA)
Michael C.K. Khoo, Ph.D.(Primary BMSR Liaison)
In critically ill preterm and term infants with cardiovascular compromise, oxygen delivery fails to meet the demand of cellular oxygen consumption, and unless recognized early and treated aggressively, failure of the circulatory system is associated with increased mortality or potentially severe short/long-term morbidity. There has been considerable progress in our understanding of developmental cardiovascular physiology, however there remains significant gaps in our knowledge particularly pertaining to treatment of patent ductus arteriosus (PDA). To address these issues, this project aims to:
- Develop a computer model for the transitional cardiovascular physiology of the neonate by modifying the adult respiratory and cardiovascular models employed in PNEUMA [2]; the neonatal model will help us gain insight into the physiological mechanisms that underlie changes in systemic and organ blood flow as a consequence of the presence of PDA.
- Examine the impact of PDA closure on hemodynamics in the neonate and the resulting effects on pulmonary and tissue gas exchange as well as respiratory control. We will also compare the relative impact of PDA closure using medication (gradual closure) versus surgical ligation (immediate closure).
Modeling of Sleep-disordered Breathing in Pediatric Obesity
Collaborative Project A3
Sally L. Davidson Ward, MD & Thomas G. Keens, MD (Project leaders)
Children’s Hospital Los Angeles (Los Angeles, CA)
Michael C.K. Khoo, Ph.D. (Primary BMSR Liaison)
Clinical studies of sleep-disordered breathing (SDB) have generally focused on upper airway collapsibility as the primary factor responsible for the development of the disorder. However, recent studies suggest that other factors that affect dynamic changes in upper airway patency, such as chemoreflex control and state dependence, also play important roles. Moreover, the pool of subjects with obesity-related SDB display a large variation of polysomnographic and clinical characteristics.
We hypothesize that this diversity in behavior results from the existence of different underlying physiological mechanisms, and that phenotyping using a quantitative dynamic model may allow us to better delineate the mechanistic differences. To test this hypothesis, we employ a minimal closed-loop model to estimate the key parameters that influence ventilatory stability in subjects during sleep. These parameters include: (a) “dynamic chemoresponsiveness”- the transfer function relating changes in alveolar PCO2 to changes in ventilatory drive; (b) the lung-to-chemoreceptor circulatory delay; (c) “plant dynamics” – the transfer function relating ventilation to alveolar PCO2; (d) the arousal threshold; (e) the arousal drive; and (f) the upper airway closing pressure. Results derived from these analyses are then used to inform the development of our structured comprehensive model of sleep, cardiorespiratory and metabolic control, PNEUMA. The knowledge derived from this study may also provide improved guidelines for customizing therapeutic strategies to individual patients.
Type 2 Diabetes: Mechanisms and Model-Based Diagnosis
Collaborative Project A4
Giovanni Pacini, Ph.D. (Project leader)
Institute of Biomedical Engineering, National Research Council (Padua, Italy)
David Z. D’Argenio, Ph.D. (Primary BMSR Liaison)
The overall goal of this ongoing Collaborative Project is to apply the novel systems modeling methods from the BMSR, to develop new diagnostic, drug development and treatment approaches for diabetes and other metabolic diseases. This will be accomplished via the following aims:
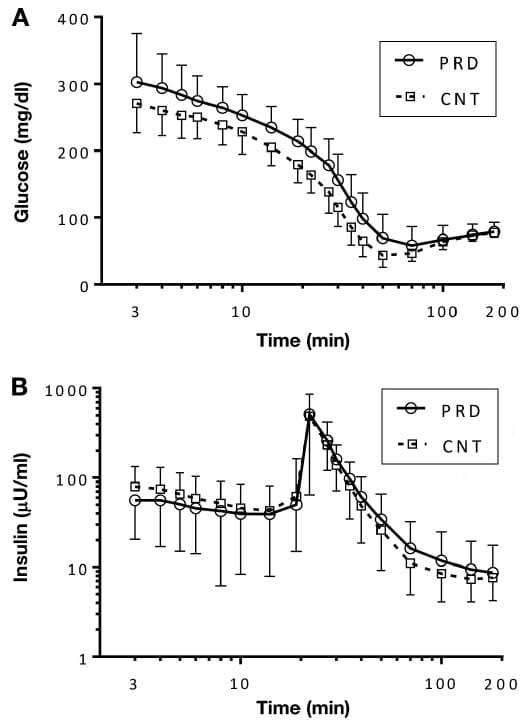
- Fully evaluate the nonparametric Laguerre-Volterra (LV) biomarkers derived from estimated insulin-to-glucose “kernels” following an intravenous glucose tolerance test (IVGTT),
utilize the extensive data base of IVGTT responses used in the earlier evaluations of the minimal model. - Using population modeling approaches, quantify the kinetics of glucagon to inform the development glucagon antagonist treatments for diabetes.
- Apply the LV modeling approach and population modeling incorporating the minimal model, to clinical trials on diabetes development and progression.